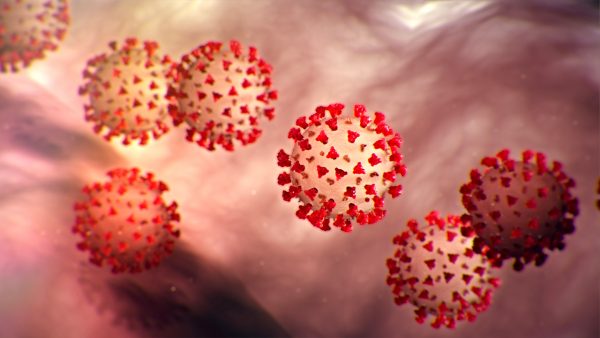
From 30 January 2020, when the first case of COVID-19 was reported, till today, March 15, 2020, the number of confirmed cases in India has risen to 107, and there have been two deaths. The government of India has reacted swiftly to this epidemic by curtailing international travel, screening those coming in from abroad and their contacts and either isolating them if they have tested positive or placing them in quarantine if they are asymptomatic. This has no doubt helped delay the epidemic. But as the government knows, the worst is yet to come.
While immediate executive action in the form of isolation of patients and quarantines, and a high pressure campaign for social distance is most welcome, this would not be sufficient if community transmission is established and the pandemic peaks. The country is particularly vulnerable because of a high degree of past neglect of public health services, and the privatization of healthcare. The country is also vulnerable because a large section of population is struggling to meet their minimum basic necessities and the last decade of economic and social policies have pushed them to the brink. In such a social and economic context, this epidemic may prove the last straw and lead to an unprecedented catastrophe unless the government pays heed to the entire charter of demands we present below.
Salient features of the COVID-19 pandemic
COVID -19 is the name of the disease caused by a particular strain of Coronavirus that has been spreading across the world. In symptoms it is remarkably similar to the seasonal flu and earlier flu and coronavirus pandemics. But it has a mortality rate much higher than the seasonal flu, though lower than the other flu and coronavirus pandemics. Over 81% of those who are infected will have only mild symptoms, another 15 % would have severe symptoms requiring medical consultation and often hospitalization and about 4 per cent would require critical care which may include ventilator support and ICU care. The mortality is highest in those above 80 and this decreases with age. Children are relatively spared.
Though it is considered unlikely that a situation like the one caused by the 1918 flu pandemic will be repeated because of better healthcare systems, it is not impossible. Neither an appropriate drug nor a vaccine is likely to become available within the next few months. Therefore the reliance is still on the age-old measures of isolation, quarantine and social distancing.
Once community transmission is established there would be a sharp increase in the number of cases, and this would be more so if there are many asymptomatic disease-spreaders or a very high susceptibility in the population. This disease could potentially infect 30 to 50% of the current adult population in the country. Even with a lower case fatality rate of 1% to critical care requirement of 4% the weakened public health systems would be overwhelmed and this would lead to millions of excess deaths in the coming year.
We do not know whether community transmission has been established, nor the actual level of spread of the disease because our current scope of testing for the virus is far too limited. In the absence of such testing, clusters of the disease- spread can develop and reach dangerous levels before they are noticed.
However there is a concern that in the name promoting social distancing, the entire burden of accountability for averting the epidemic and preventing loss of life due to it is shifted to the people and within that, the most vulnerable sections. The current approach to pandemic control that leads to shutting down of considerable economic and social activity is unsustainable and at best of temporary benefit. The epidemic peak may occur months later, and not now. Such a delay, or flattening of the epidemic curve as it is known, is useful because it would give time to the government hospitals time to gear up. But if no efforts are made to prepare the hospitals or expand the testing, the delay only leads to prolonged economic and social suffering of the majority with adverse health outcomes deferred but not averted.
The main thing that communities can do is to protect themselves by rapid improvements in health related practices and hygiene. Communities also need to extend solidarity with those who are suffering health-wise or economically due to the epidemic. Peopless movements recognize the role they have in both promoting hygiene and in building solidarity.
We call on national and state governments to address both the adverse health outcomes and the adverse impact the control measures are making on the lives and livelihoods of people which are as equally damaging and require mitigation.
A Peoples Charter of Demands – Save Lives, Save Livelihoods and Respect Human Rights
Based on the understanding that is discussed above (and elaborated in a background paper on the COVID-19 epidemic), the Peoples Science Movements and the Peoples Health Movement adopt the following charter of demands that articulates its understanding and its demands:
Health Care Related
1. Government must expand testing facilities and criteria for COVID-19. Testing should not be limited to only those with symptoms who have travelled to certain countries and those who have come in contact with them. Any clinically suspected person should be able to get tested. While containment by isolating patients with the disease, tracing contacts, and quarantining individuals returning from nations with an established outbreak may continue to be relevant for a longer period, the system needs to gear up for addressing community transmission.
2. Government must rapidly prepare public health services for a surge in patients requiring healthcare and hospitalization by strengthening the public hospitals. This would require, at the very least, one hospital with an ICU; potential isolation wards and ventilators; and oxygen supply in every five to ten lakh population. It would also require corresponding improvement in supply of relevant medicines and consumables such as oxygen and deployment of human resource. We reiterate that such an expansion was anyway long overdue, and this epidemic is an opportunity to rush such preparation through.
3. In the event that the pandemic becomes a full blown emergency in any part of the country, it would be necessary that all existing medical facilities be brought under a centralised district authority, including all private hospitals. Allocation of medical facilities will have to be done by this authority and not by the market mechanisms. The protocols and administrative and financial measures required for doing so must be put in place as part of epidemic readiness.
4. Immediate strengthening of the Integrated Disease Surveillance Programme, by a major increase in capacity to test for this disease, and to report on all seasonal flu and other fever related deaths from across all facilities – public and private. In the absence of such expansion, we caution that the country could even go through an epidemic without knowing it, or could be surprised by large cluster-outbreaks where they are least expected.
5. As a long term measure we call for establishing a Government Centre for Disease Control in every district which is staffed and facilitated to test, identify and provide alerts and advice precautionary measures for pathogenic attacks like the current COVID-19 pandemic.
6. Ensure safe working conditions and adequate protective equipment for healthcare and support staff. These are to be provided not only in hospitals but also for frontline workers supporting home quarantine and isolation. This would require that medical tools such as effective facemasks and sterilizing fluids are prioritized for front-line healthcare workers and patients.
7. Ensure that the distribution of scarce resources in the event of a widespread outbreak should be governed by a clear evaluation of the public health needs, rather than on sales to the highest bidder (this problem emerged with Oseltamivir (Tamiflu) during the 2009 H1N1 influenza pandemic). International collaboration vis-a-vis developments in medication and vaccines is a must, and care must be taken to prevent patent monopolies from limiting production of potential treatments.
Social Distancing and Human Rights
8. Social distancing must necessarily be done by public education and persuasion. The use of coercive measures would be unfair and unhelpful. Mass gatherings, public events, whether social, religious, sports related, cultural or political, could be dissuaded for some time more- but should not be banned.
9. Active community support and outreach services need to be built up for those in home quarantine, those whose social security benefits are curtailed due to closure or those having difficulties in accessing essential services. Many under home quarantine will have co-morbidities that would require access to follow up care and medication. Many children will need access to supplementary nutrition programs, more so, when their parentss livelihood is compromised. Shutting down such services without providing for alternatives would be unfair.
10. When populations are placed under lockdown or quarantine, special measures would need to be in place to ensure that this is done in a humane manner and without abuse to core human rights. Governments need active engagement of human rights institutions and civil society organizations and trade unions to inspect and report back on standards of care and the problems that the most vulnerable sections are facing.
11. The freedom of the media to report on the epidemic and its consequences must be safeguarded at all times. However when carrying messages on the nature of spread, the source of infection or on treatment, news media must be encouraged to keep to the parameters set by government channels, international health institution channels, or of universities and research institutions. Where information is from any other sources, the news must be accompanied by a disclaimer that this is unverified and could be fake. Any blanket ban on media freedoms is unwarranted and should be resisted.
Redressing Economic Inequity – As Cause and Consequence
12. Maintenance of routine economic activity, which primarily means safeguarding of the livelihoods of the majority, should also be acknowledged and acted upon as a public health priority. Public education should also address the need to build solidarity in such times. The working people and poor take a much larger economic hit due to disruption of livelihoods than the salaried section and the affluent, and this should be acknowledged. There has to be active community support and support from employers to those in home quarantine and those whose livelihoods are compromised by these lockdowns.
13. There must be an immediate increase in public expenditure that leads to widespread demand-side support in the form of increased social security and food security measures such as enhancement of entitlement under the Public Distribution System (PDS), and cash transfers. This is urgently required to address the attack on livelihoods of the majority that have already been compromised by a decade of economic policies that intensified capital accumulation, but destroyed livelihoods. Further concessions to corporate industry to counter the crisis they are also facing, and further austerity for the working people would be most counter-productive and iniquitous.